Would it be possible for diabetic patients to control their blood sugar levels with a better diet alone, without using any medicines? A recent study suggests this might be true for some patients with mild diabetes.
The concept of reversing diabetes might be news for you as a diabetic patient, but don’t worry; it is as much news for you as it is for medical doctors. Despite anecdotal and observational evidence of diabetes reversal, the medical community has been, at large, evading the obvious. But not anymore. A healthy lifestyle revolution, predominantly orchestrated by health gurus on social media, and the resulting improvement in the lives of many chronic disease patients have made it inevitable that doctors scrutinize this subject under the lens of research.
One such study on diabetic patients came out in the last week of October 2024, addressing a few critical questions about the basics of diabetes reversal while raising many minor ones related to the disease, race, and lifestyle.
This blog post about the research in question has two parts. The first part will take you through the actual research, in as simple a language as I could achieve, which will still be as painful to read as it was to write. But if you find this part hard to digest, you are welcome to skip it and jump directly to the second part, the main message of the research for the doctors and the patient, simple bits of practical advice that one can use as a guide to navigating one’s diabetes reversal journey.
Details of the research
Who were the patients?
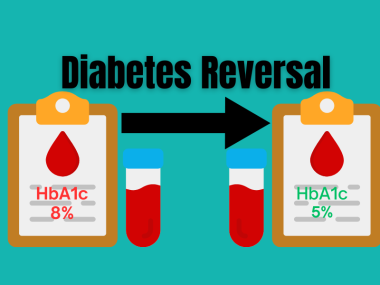
Researchers enrolled sixty-five Type 2 diabetic patients who were managing their disease with medicine alone. No one was on insulin. All of them had diabetes for less than ten years and HbA1c of less than 8%. Eight people dropped out of the study, primarily due to non-adherence. The final study population was 57 patients, 37 African Americans and 20 European Americans.
What was the purpose of the study?
Researchers wanted to know whether a low-carbohydrate diet alone, independent of weight loss, had any effect on the functioning of the pancreas and insulin sensitivity.
What did the patients do?
After discontinuing their diabetes medicines for 2 weeks, the patients were assigned either a low-carbohydrate diet (only 9% of daily calories) or a higher-carbohydrate diet (55% of total calories). I would hasten to add that this “higher-carbohydrate diet” is essentially the regular diet for an average person in the United States.
The total daily calorie intake for each patient was kept at a weight-maintaining level, for this was the said purpose of the research: to study the effects of a low-carbohydrate diet alone, without any changes in weight.
They measured the insulin-secreting capacity of these patients at the start of the study and after being on specific carbohydrate diets for twelve weeks. In addition, the scientists also measured insulin sensitivity on both occasions, the beginning and the end of the study.
How did they measure insulin secretion?
Insulin is secreted by specific cells in the pancreas called Beta cells. In other words, insulin secretion is a measure of pancreatic beta-cell function: normal insulin secretion implies good-functioning beta cells; in contrast, less-than-normal insulin secretion indicates beta cell failure.
The researchers used a hyperglycemic clamp, meaning infusion of glucose through a vein to raise the blood glucose levels to a certain target, to measure the insulin-secreting capacity of these patients at baseline and after using a low-carbohydrate diet for 2 weeks. Since insulin is secreted by the pancreas in two phases, the scientists measured both phases of insulin secretion: an acute phase that begins immediately after glucose ingestion and lasts for about 30 minutes; and a second phase that begins concurrently with the acute phase but lasts longer, up to 2 to 3 hours.
Why and how did they measure insulin sensitivity?
Since type 2 diabetes stems from a combination of loss of insulin-secreting capacity of the pancreas and increased insulin resistance, it is imperative to incorporate the measurement of insulin sensitivity into the assessment of insulin secretion.
To achieve this, the researchers used an oral glucose tolerance test, again at baseline and after twelve weeks, and measured the Disposition Index, a marker of beta cell function that factors in insulin secretion and sensitivity.
What did the results of the study show?
After 12 weeks, the acute phase of insulin secretion was twice as high with a carbohydrate-restricted diet than with a high-carbohydrate diet. This difference was significant in 37 African Americans but not European Americans.
The second-phase insulin response, also called maximal response, was 22% greater with the low-carbohydrate diet. This increase in insulin secretion due to a low-carbohydrate diet was significant in European Americans but not African Americans.
Both diets showed no significant change in insulin sensitivity.
Message of the research
A low-carbohydrate diet can reverse type 2 diabetes
This study shows that a carbohydrate-restricted diet, without any changes in total daily calorie intake or weight, has “beneficial effects” on beta cell function. Simply put, if you take a low-carbohydrate diet, your pancreas starts producing more insulin in as little as twelve weeks.
What causes type 2 diabetes?
You might be wondering, “How?” But to understand that we first need to know what causes type 2 diabetes in the first place. Type 2 diabetes results from some combination of decreased insulin production by the pancreas and increased insulin resistance in the body. While the mechanisms behind insulin resistance are complex and poorly understood, the changes in the pancreas that lead to decreased insulin production are well-studied.
Decreased insulin production in type 2 diabetes is due to beta cell failure, which results from two processes: the reduced ability of beta cells in glucose sensing and responsiveness, also called glucose blindness, and beta cell apoptosis, meaning death.
A low-carbohydrate diet increases insulin secretion
A decrease in acute-phase insulin secretion occurs primarily due to the loss of glucose-sensing ability of the beta cells of the pancreas. This loss of glucose sensing occurs early on in type 2 diabetes and is attributed to glucose toxicity and the proinflammatory markers released from a fatty liver. In this study, just two weeks of a low-carbohydrate diet doubled the acute-phase insulin secretion, the only explanation of which can be an increase in the glucose-sensing capacity of beta cells.
The loss of second-phase results, on the other hand, from beta cell death. The beta cell death is triggered by a proinflammatory milieu created by fat cells in the pancreas. A low-carbohydrate diet decreases this inflammation in the pacnreas and starts instead the process of repair and regeneration, and that is perhaps what happened to the patients in this study. In a similar two-year-long study, a low-carbohydrate diet led to the normalization of second-phase insulin response, suggesting the possibility that beta cell death could be reversed if given enough time. Or could it be that the apparently dead beta cells are not actually dead—they just go dormant?
Different ethnicities may respond differently
Then, the research revealed a few race-related traits of type 2 diabetes, pointing to the possibility that varying mechanisms underly type 2 diabetes in different ethnicities, supporting the previous research, which contends that there exist inherent biological differences in the mechanism of beta cell failure between races.
How this research helps your reverse your diabetes?
Moving from research to real life, the question is, “Is this low-carbohydrate business practical for a layperson?” I say yes. And I do not draw my optimism from the results of this study (this research provides scientific evidence of what is actually happening to our patients’ bodies). My optimism originates from many committed patients’ success in reversing their diabetes with minimal support. Our clinic patients never received “packaged groceries” as the subjects in the research did; our patients did not always have a certified dietician who watched their calories and weight; they did not even have a basic understanding of protein, carbohydrates, and fats. Still, many of them achieve complete remission.
My point is that if patients in a third-world country like Pakistan, despite its limited resources of medical and health facilities and even more limited interest of the population in these resources, can reverse their diabetes, the journey for patients in wealthy countries should be way more manageable and practical.
You don’t need extreme diets to reverse your diabetes!
Lastly, we need to bust a big myth. When it comes to diabetes reversal or weight loss diets, you are given to believe that form of extreme change in your daily food. It is either some form of keto diet consisting of a big chunk of fats providing more than 65% of your daily calories, as was the case in this study. Or meals should mainly be proteins with some fats. But it is an illusion created by some health experts whose own diabetes reversal journey might have required such extreme measures and who now believe that there exists no other path to this end.
My experience with my patients shows otherwise. As far as these extreme diets are concerned, I agree with the critics of diabetes reversal that continuing such diets without the supervision of an expert is not only impossible but extremely dangerous. However, not all diabetic patients need such radical changes. A simple, balanced diet should suffice, with the only significant change of replacing refined carbohydrates with complex carbohydrates. The diabetes reversal outcomes of this balanced diet can be bolstered further by adding other healthy habits of regular exercise, good sleep, and stress management.
Take Home
That a low-carbohydrate diet has beneficial effects for diabetic patients has become an established fact. This study helped us understand the scientific basis of these benefits. We all know that no drug—oral medicines or subcutaneous insulin—has ever been shown to improve the functioning of the pancreas. Such transformation did occur in this study using a low-carbohydrate diet for as little as 2 weeks. With the impending crisis of metabolic syndrome and diabetes, such research provides huge support to the work of those doctors who are helping their patients to reverse their diabetes and metabolic syndrome. Have you begun the journey of reversing your diabetes yet?