Telemedicine, also known as telehealth or virtual health, saw a sharp surge during the COVID-19 pandemic. This trend lately seems to dwindle, prompting many governments across the globe to take sincere steps in support of telehealth. The United States is constantly working to make structural changes in the payment for virtual visits. The European Parliament and the European Council announced the EU4Health program, an initiative that will allow the sharing of digital health records, e-prescriptions, and telehealth in general. Middle eastern countries are developing cellular apps to make the healthcare system more accessible. Is this race to promote telemedicine just a new trend that all well-off countries are following to win some game? Or whether all responsible governments, those who value the health and happiness of the people, see telehealth as an unprecedented opportunity to improve their citizens’ health? Why is telehealth gaining so much attention? Can it be of any help to a resource-strained country like Pakistan?
Table of Contents
Benefits of Telehealth
Telehealth brings four major benefits to any healthcare: accessibility, equity, affordability, and economy.
These advantages of virtual health make it even more attractive and beneficial for developing countries like ours. But, alas! Neither our government nor the private sector has paid much attention to telehealth, missing an opportunity that can revolutionize the health of our patients. If used appropriately, it can revolutionize our healthcare with no high upfront cost. Better still, it would bring in savings and prosperity for all parties. For some in the form of money, for others in the form of health, and for all the joy of doing something that makes this world a better place. Let’s see how!
Accessibility
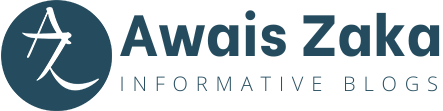
The majority of our patients don’t have access to the healthcare system. Much of our population still lives in villages, sometimes so remote that they must travel dozens of miles to visit even a basic health unit. As for tertiary level care, it remains beyond the reach of even urban dwellers. This problem of access to healthcare affects every segment of society, and our traditional methods of delivering healthcare fail to offer anything but a disappointment. To this access problem, telemedicine provides a far better solution. Virtual technology allows connecting patients with the healthcare system from the comfort of their homes using cell phones. This connectivity is now possible because mobile networks have reached far into the peripheries, and almost every house in Pakistan has at least one phone, many of which are smartphones. However, establishing this connection and having the patient learn and trust this digital version of medical practice may need to be phased out. Of course, initially, there will be reluctance, even resistance, but once patients start seeing the benefits, many will not only welcome but prefer to manage their health via virtual tools. Beyond this primary everyday care, telehealth has more to offer. At the next level, this technology can connect the patients at basic and district health units with the experts in the tertiary care centers. Meeting the expert virtually, patients requiring a visit to tertiary care can start the consultation online, an opportunity for both to know each other before an in-person interview. Such tele-visits have shown to be very helpful in building trust and rapport with the patients, making future in-person meetings not only more productive but meaningful.
Equity
Distance is not the only factor that creates healthcare disparities. Socio-economic and educational inequality—a sad reality that is sharper and clearer the poorer a country is—almost always entails inequity in access to healthcare. Most patients struggle with everyday health concerns, like sore throat, diarrhea, or even a headache. And when it comes to chronic issues, like high blood pressure, diabetes, or kidney and heart disease, which require life-long medication, periodic tests, and regular follow-ups, even well-off patients give up. Our vast inequality leaves only a minority with the privilege of full-fledged access to health care. Consequently, the rich have access to MRI for their tension headache, while the poor die of colon cancer without leaving their quacks threshold. Virtual health can help address these disparities. Using telehealth can significantly cut the cost of transport, removing a significant barrier for the patients toward better health. This availability of healthcare would encourage the patients to use the mainstream healthcare system rather than quacks or herbalists. Furthermore, it will increase the follow-up rates for those who struggle with their poorly managed disease because they cannot afford transport to or stay in the big city where they often have to go to manage disease complications. This way, telehealth can significantly ease the burden of healthcare costs to a patient by cutting the transport expenses and better managing chronic diseases, dramatically reducing the need for hospitalizations and saving thousands of rupees in costs.
Affordability
Thus, solving the issues of accessibility and disparity, virtual health can make healthcare for a significant part of our population more affordable. However, it may do so indirectly. Practically speaking, many don’t approach mainstream healthcare, not because of the actual cost but rather the fear of cost. The perception is real, but it springs from exaggerated and misleading numbers that stem from the tertiary level care, which is expensive everywhere, not just in Pakistan, and which should not be the face of healthcare, as it is in Pakistan. In fact, if we look at primary care in Pakistan, it is so cheap that any argument for its being expensive seems illogical. For example, essential medications for chronic conditions like high blood pressure, heart conditions, and diabetes are dirt cheap, most of them not even more than five to ten rupees per pill. It is safe to say that a well-managed hypertensive and diabetic patient can buy his monthly prescription within the range of 4000 to 6000 PKR. Then, the fee for primary care physicians is in the range of 200 to 700 PKR. A visit to a consultant, which should only be the case for five to ten percent of the population and should not be more than four per year, costs 1500 to 4000 PKR. Similarly, basic labs—blood count, kidney function, liver function, and urinalysis—run in thousands, a set that a well-managed patient requires only a few times a year. In other words, the patient’s fears are misplaced, requiring a massive realignment to bring them to accept modern medicine’s authenticity and sincerity. Telemedicine may not reduce the cost of a medication or a blood test. Still, by removing the barriers like distance, transport, and lack of availability, in short, by bringing the patient to the mainstream healthcare system, where his condition is evaluated and managed timely, it can make the healthcare more affordable.
Economy
An excellent healthcare system is not the one that provides just the best care but rather one which provides the best possible care at the minimum cost, both to the patient and the state. How can telemedicine turn our healthcare into an economical one? By making healthcare more accessible and affordable, telemedicine carries the potential to bring in huge savings. When patients start approaching the healthcare system on the first appearance of a symptom, without the fear of cost or distance, they have better chances of early diagnosis, better treatment, and good outcomes, all of which keep the patient healthy. For the patient, this results in fewer disease complications, fewer emergency room visits, fewer hospitalizations, fewer sick days off work—and overall better health. For the state, such a healthcare system means less spending on a disease and its complications, which leads to huge savings, an amount that can then be diverted to more meaningful objectives like education and employment, building a healthy and prosperous community.
Telehealth Potential
In a word, telehealth has massive potential for bridging the gaps in our healthcare system, gaps that seem impervious to any other solution. Lowering medical costs and maximizing the health of our citizens can best be achieved by tele-delivered healthcare. The covid pandemic has highlighted this latent opportunity and its potential for healthcare delivery. True, the barriers like regulations, payment plans, and, most importantly, patient acceptance stand tall and wide. Still, it is our job to get over these barriers and bring telemedicine from the sideline to the core of the healthcare system, where it belongs. With such bright prospects and all the gadgets available, what is holding us back from using telehealth? It is time we equip our clinics and hospitals with telehealth tools and make the routine use of the advanced technology to make our healthcare accessible and affordable for as large a population as possible.